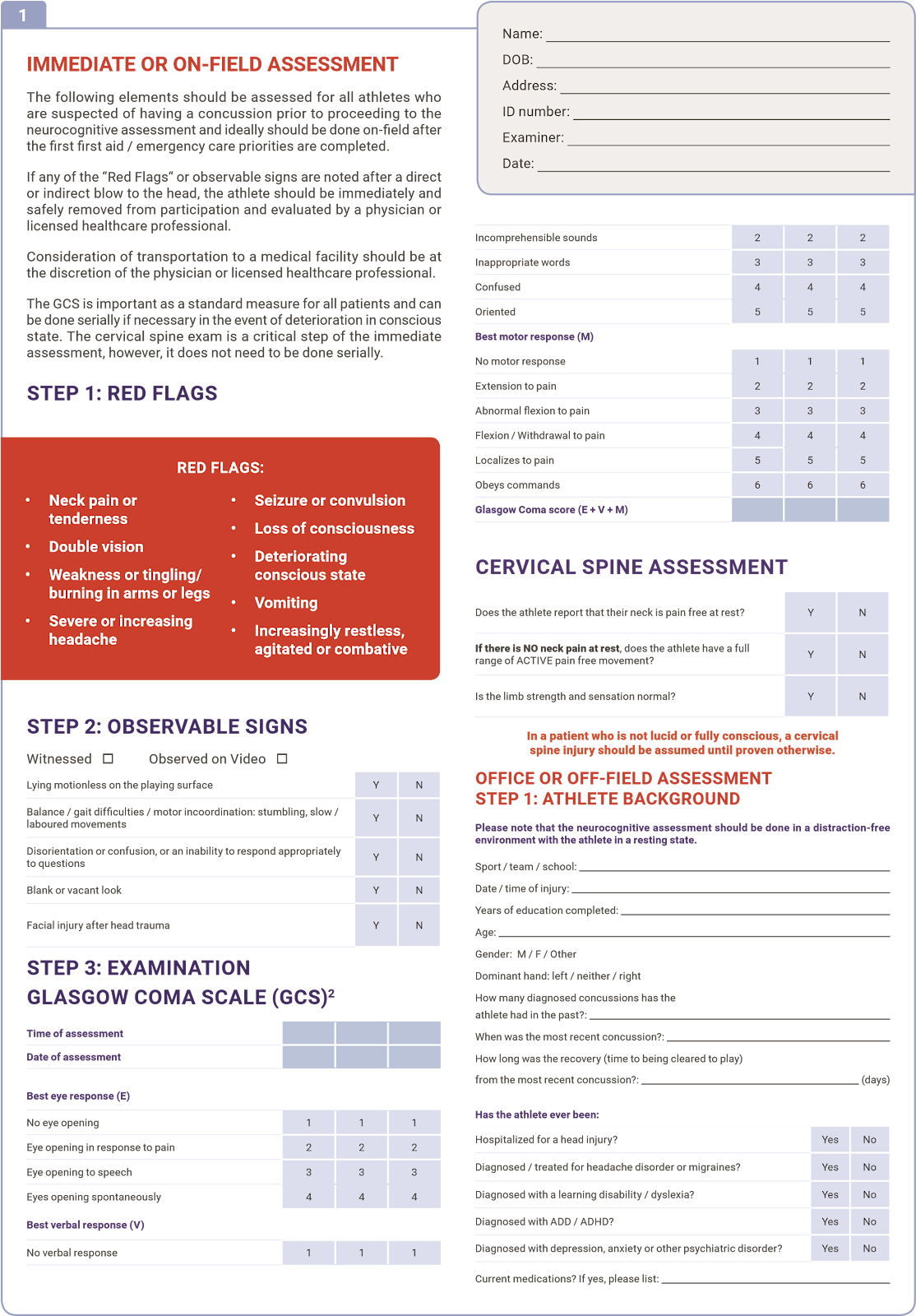
• Concussion can be defined as a brain injury that arises from trauma to the head, neck or through an impulsive force transmitted to the head from elsewhere in the body • Concussion results in a disturbance of brain function and should be treated as a serious and significant injury with potentially fatal consequences • The presence of a brain or spinal injury should always be considered in a player who is apparently concussed
• ANY PLAYER WITH A CONCUSSION OR A SUSPECTED CONCUSSION SHOULD BE REMOVED FROM THE FIELD OF PLAY IMMEDIATELY AND SAFELY AND SHOULD NOT RETURN TO PLAY, TRAINING OR OTHER PHYSICAL ACTIVITY ON THE SAME DAY
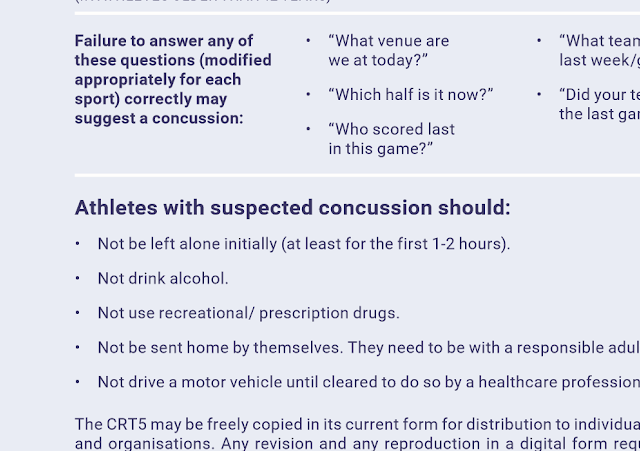
• A player does not need to lose consciousness to be concussed • The common symptoms of concussion include headache, dizziness, memory loss, disturbance of balance • The onset of symptoms can occur over minutes but can be delayed for hours • All coaches, parents and referees should familiarize themselves with the pocket Concussion Recognition Tool (CRT5) to assist in identifying concussion. (appendix 1) • All doctors, physiotherapists and paramedics should familiarize themselves with the CRT5 and with SCAT5 and Child- SCAT5 to assist in identifying concussions (Appendix 2 and 3) • Concussed players should not be left alone • Concussed players should not drive, should not take alcohol and should be escorted home • Most concussions (80-90%) resolve over a 7-10 day period but may persist for considerably longer • It is very important to note that the symptoms of concussion in children and adolescents can be prolonged and it is not uncommon in certain circumstances for them to last for several weeks or months
• All players who suffer a concussion should be referred to a medical practitioner
• Concussed players should not return to play, training or other physical activity while symptoms persist
• Return to sport guidelines must follow a stepwise progression (appendix 4). ▪ There should be a graded return to training activity
▪ There should be at least 24 hour (or longer) for each step of the RTS progression ▪ A period of 24-48 physical and cognitive (mental) rest is recommended before beginning the return-to-sport (RTS) progression ▪ Physical and mental activity can be progressively increased provided that it doesn’t worsen or bring on symptoms
• Medical clearance is necessary before a player who suffered a concussion can return to play
• Children and adolescents should not return to any activity until they have made a successful return to school/college • Consideration should be given to a stepwise return-to-school programme for children and adolescents when symptoms persist
KEY CONSIDERATIONS
- Any player with a concussion or a suspected concussion should be removed from the field of play, immediately and safely, and should not return to play, training or other physical training on the same day
- All players who suffer a concussion should be referred to a medical practitioner
- Return-to-sport (RTS) guidelines must follow a stepwise progression
- Medical clearance is necessary before a player who suffered a concussion can return to play
Note: These guidelines are based on the Consensus Statement from the 5th International Conference on Concussion in Sport, Berlin, October 2016 (published April 2017)
on May 11, 2017 – Published by
BJSM Online First, published on April 28, 2017 as 10.1136/bjsports-2017-097508CRT5
© Concussion in Sport Group 2017
1 Copyright Article author (or their employer) 2017. Produced by BMJ Publishing Group Ltd under licence.
BJSM Online First, published on April 26, 2017 as 10.1136/bjsports-2017-097506SCAT5
To download a clean version of the SCAT tools please visit the journal online (http://dx.doi.org/10.1136/bjsports-2017-097506SCAT5)
WHAT IS THE SCAT5?
The SCAT5 is a standardized tool for evaluating concussions designed for use by physicians and licensed healthcare professionals1. The SCAT5 cannot be performed correctly in less than 10 minutes.
If you are not a physician or licensed healthcare professional, please use the Concussion Recognition Tool 5 (CRT5). The SCAT5 is to be used for evaluating athletes aged 13 years and older. For children aged 12 years or younger, please use the Child SCAT5.
Preseason SCAT5 baseline testing can be useful for interpreting post-injury test scores, but is not required for that purpose.Detailed instructions for use of the SCAT5 are provided on page 7. Please read through these instructions carefully before testing the athlete. Brief verbal instructions for each test are given in italics. The only equipment required for the tester is a watch or timer.
This tool may be freely copied in its current form for distribution to individuals, teams, groups and organizations. It should not be altered in any way, re-branded or sold for commercial gain. Any revision, translation or reproduction in a digital form requires specific approval by the Concussion in Sport Group.
Recognise and Remove
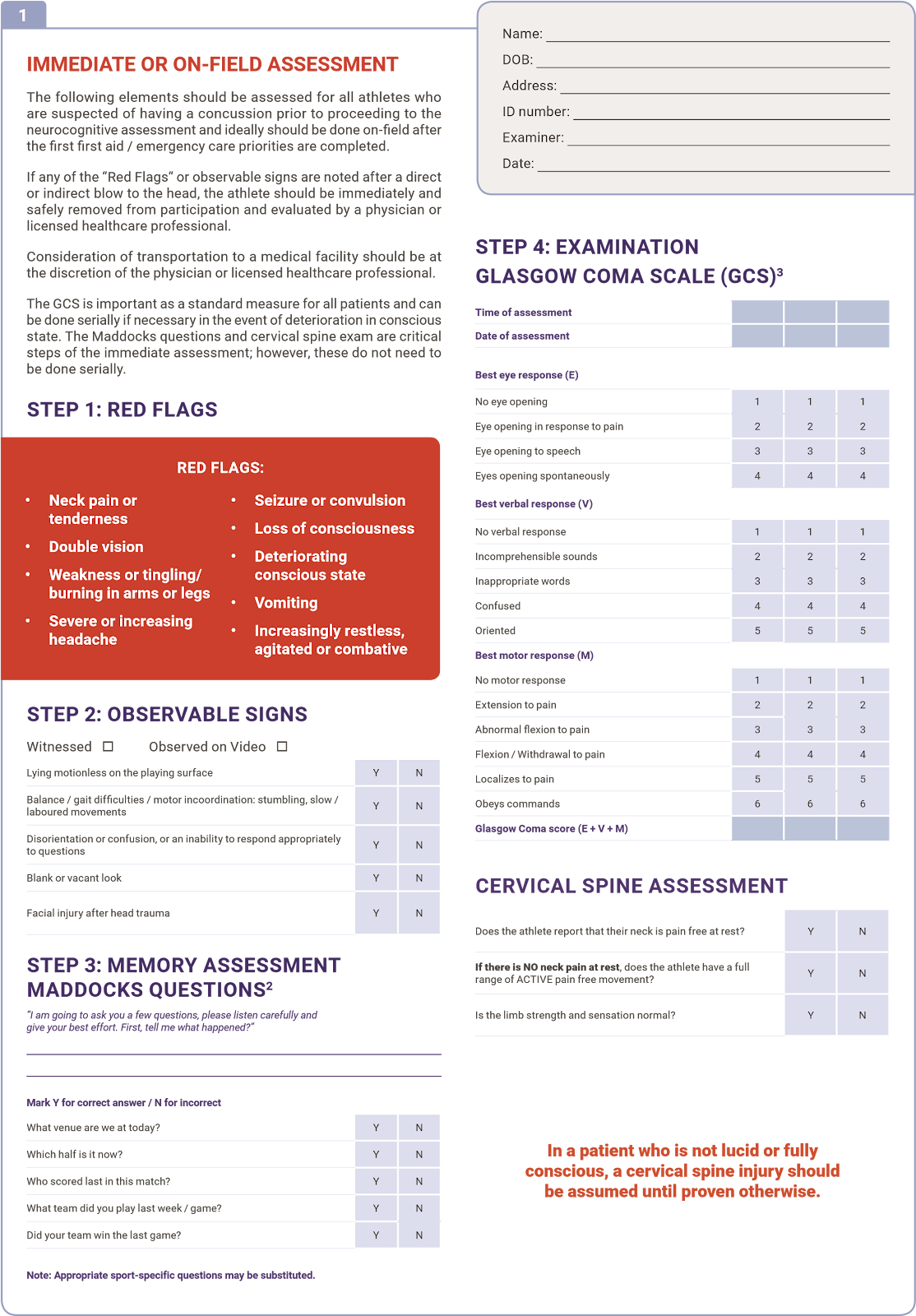
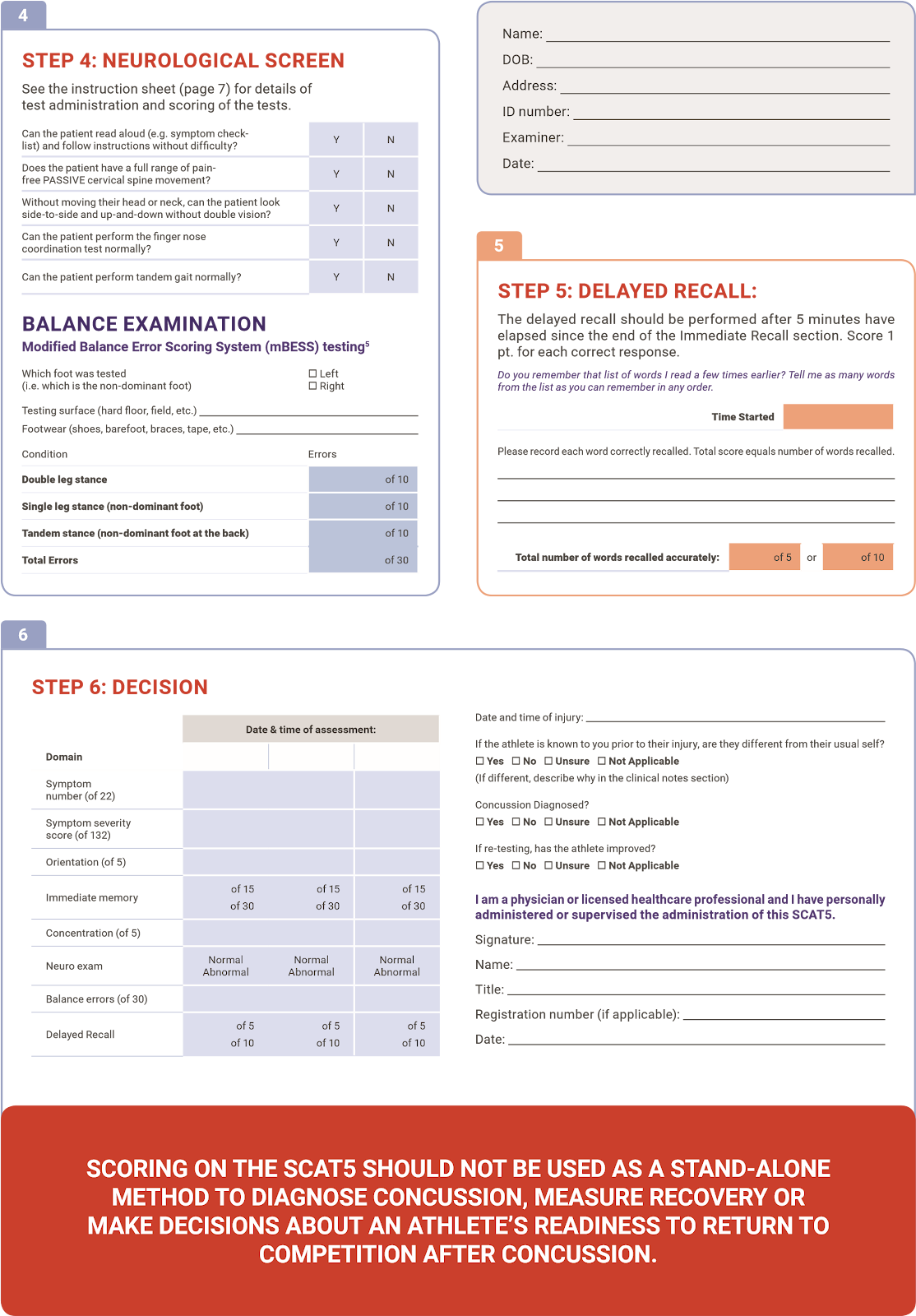
A head impact by either a direct blow or indirect transmission of force can be associated with a serious and potentially fatal brain injury. If there are significant concerns, including any of the red flags listed in Box 1, then activation of emergency procedures and urgent transport to the nearest hospital should be arranged.
Key points
- Any athlete with suspected concussion should be REMOVED FROM PLAY, medically assessed and monitored for deterioration. No athlete diagnosed with concussion should be returned to play on the day of injury.
- If an athlete is suspected of having a concussion and medical personnel are not immediately available, the athlete should be referred to a medical facility for urgent assessment.
- Athletes with suspected concussion should not drink alcohol, use recreational drugs and should not drive a motor vehicle until cleared to do so by a medical professional.
- Concussion signs and symptoms evolve over time and it is important to consider repeat evaluation in the assessment of concussion.
- The diagnosis of a concussion is a clinical judgment, made by a medical professional. The SCAT5 should NOT be used by itself to make, or exclude, the diagnosis of concussion. An athlete may have a concussion even if their SCAT5 is “normal”.
Remember:
- The basic principles of first aid (danger, response, airway, breathing, circulation) should be followed.
- Do not attempt to move the athlete (other than that required for airway management) unless trained to do so.
- Assessment for a spinal cord injury is a critical part of the initial on-field assessment.
- Do not remove a helmet or any other equipment unless trained to do so safely.
© Concussion in Sport Group 2017
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
Copyright Article author (or their employer) 2017. Produced by BMJ Publishing Group Ltd under licence.
CONCUSSION INJURY ADVICE
(To be given to the person monitoring the concussed athlete)
This patient has received an injury to the head. A careful medical examination has been carried out and no sign of any serious complications has been found. Recovery time is variable across individuals and the patient will need monitoring for a further period by a responsible adult. Your treating physician will provide guidance as to this timeframe.
If you notice any change in behaviour, vomiting, worsening headache, double vision or excessive drowsiness, please telephone your doctor or the nearest hospital emergency department immediately.
Other important points:
Initial rest: Limit physical activity to routine daily activities (avoid exercise, training, sports) and limit activities such as school, work, and screen time to a level that does not worsen symptoms.
- Avoid alcohol
- Avoid prescription or non-prescription drugs without medical supervision. pecifically: a) Avoid sleeping tablets
b) o not use aspirin, anti-inflammatory medication or stronger pain medications such as narcotics
- Do not drive until cleared by a healthcare professional.
- eturn to play sport re uires clearance by a healthcare professional.
Clinic phone number:
Patient’s name: ate time of injury:
ate time of medical review:
Healthcare Provider:
| INSTRUCTIONS Words in Italics throughout the SCAT5 are the instructions given to the athlete by the clinician |
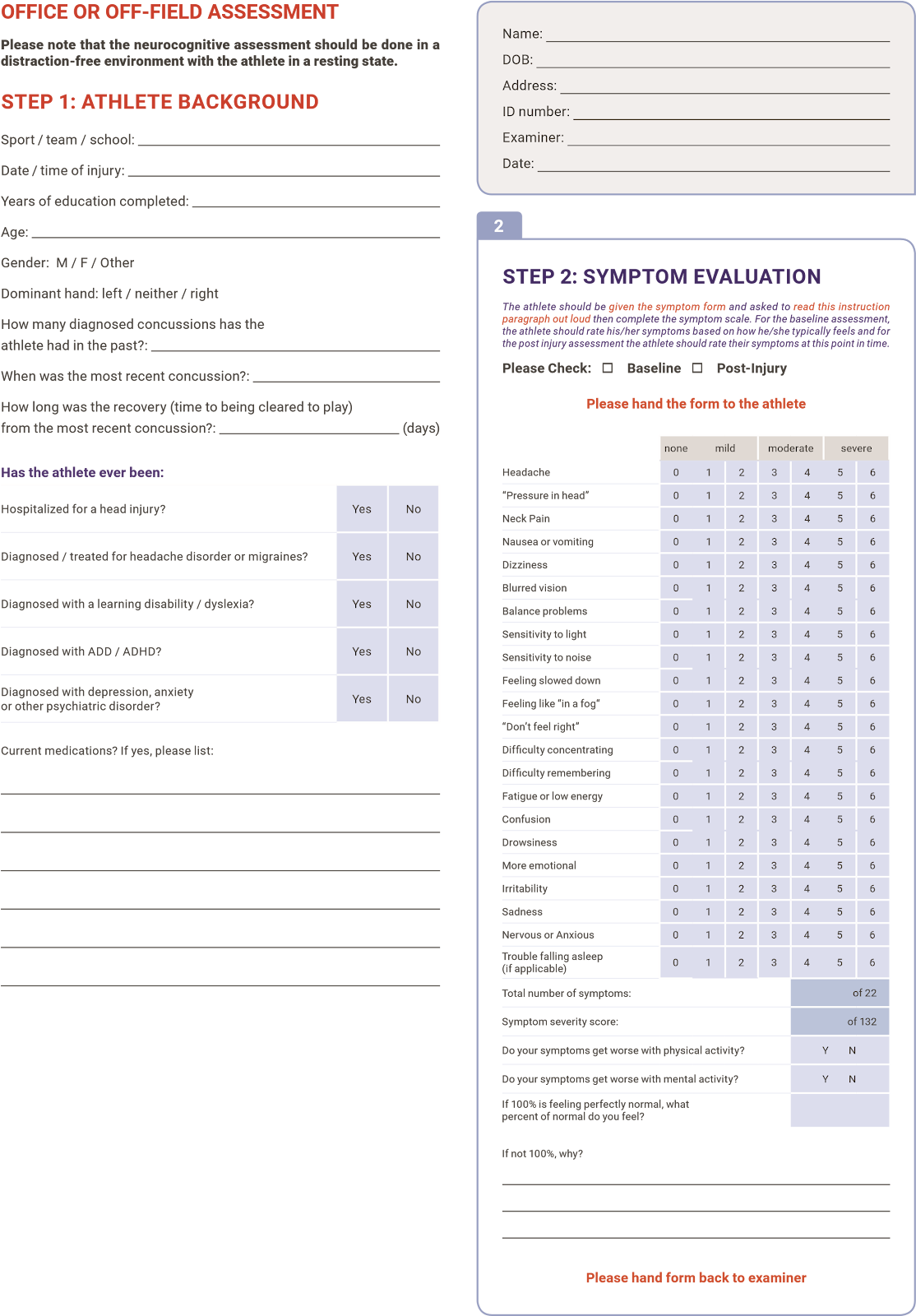
Symptom Scale
The time frame for symptoms should be based on the type of test being administered. At baseline it is advantageous to assess how an athlete “typically” feels whereas during the acute post-acute stage it is best to ask how the athlete feels at the time of testing.
The symptom scale should be completed by the athlete, not by the examiner. In situations where the symptom scale is being completed after exercise, it should be done in a resting state, generally by approximating his her resting heart rate.
or total number of symptoms, maximum possible is except immediately post
injury, if sleep item is omitted, which then creates a maximum of 1.
or ymptom severity score, add all scores in table, maximum possible is x 1 , except immediately post injury if sleep item is omitted, which then creates a maximum of 1x 1 .
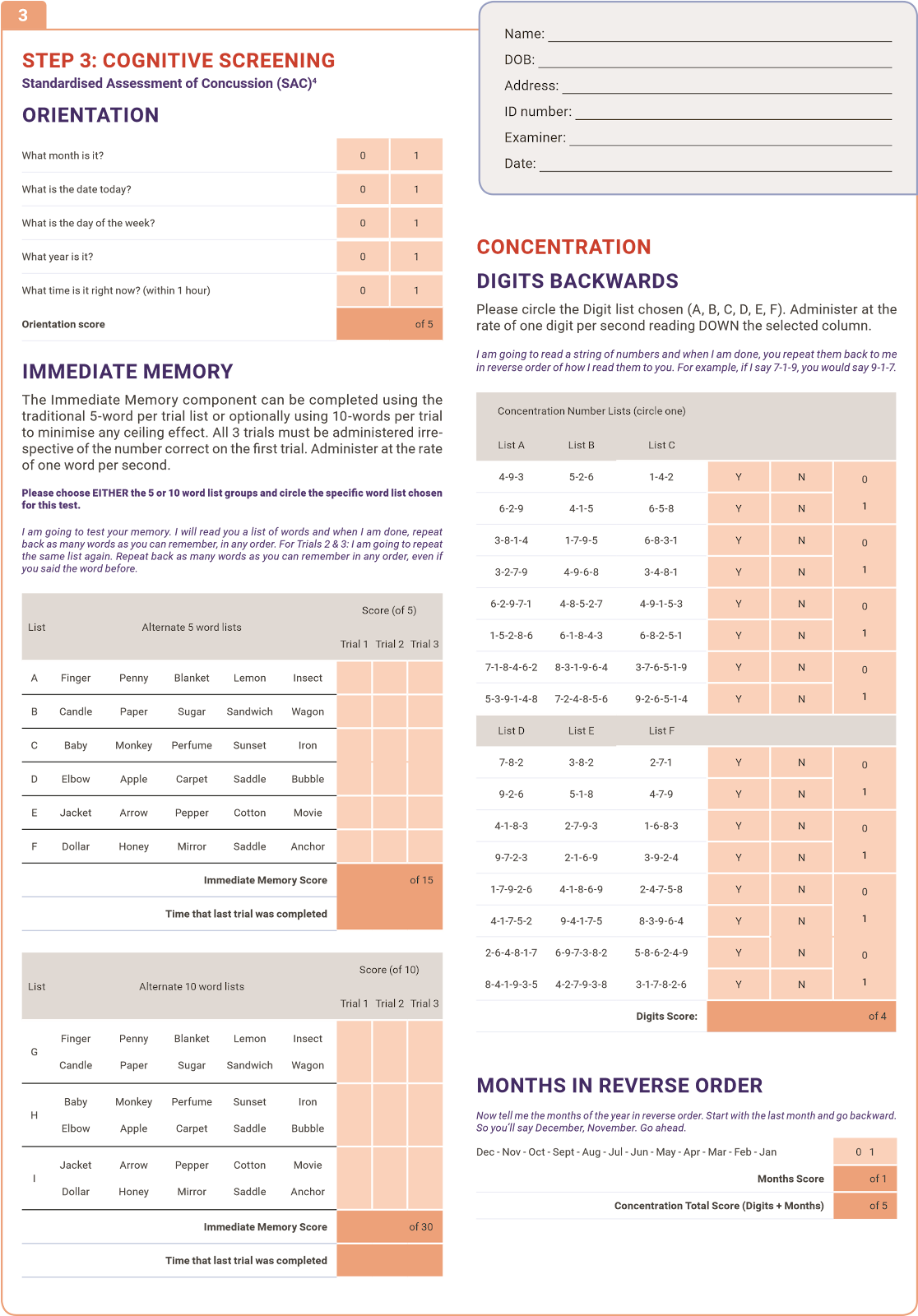
Immediate Memory
The Immediate Memory component can be completed using the traditional 5-word per trial list or, optionally, using 10-words per trial. The literature suggests that the Immediate Memory has a notable ceiling effect when a 5-word list is used. In settings where this ceiling is prominent, the examiner may wish to make the task more difficult by incorporating two word groups for a total of 1 words per trial. In this case, the maximum score per trial is 1 with a total trial maximum of .
Choose one of the word lists (either 5 or 10). Then perform 3 trials of immediate memory using this list.
Complete all 3 trials regardless of score on previous trials.
“I am going to test your memory. I will read you a list of words and when I am done, repeat back as many words as you can remember, in any order.” The words must be read at a rate of one word per second.
Trials 2 & 3 MUST be completed regardless of score on trial 1 & 2.
Trials 2 & 3:
“I am going to repeat the same list again. Repeat back as many words as you can remember in any order, even if you said the word before.“
Score 1 pt. for each correct response. Total score equals sum across all 3 trials. Do NOT inform the athlete that delayed recall will be tested.
Concentration
Digits backward
Choose one column of digits from lists A, B, C, D, E or F and administer those digits as follows:
Say: “I am going to read a string of numbers and when I am done, you repeat them back to me in reverse order of how I read them to you. For example, if I say 7-1-9, you would say 9-1-7.”
Begin with first digit string.
If correct, circle for correct and go to next string length. If incorrect, circle for the first string length and read trial in the same string length. ne point possible for each string length. Stop after incorrect on both trials (2 N’s) in a string length. The digits should be read at the rate of one per second.
Months in reverse order
“Now tell me the months of the year in reverse order. Start with the last month and go backward. So you’ll say December, November … Go ahead” 1 pt. for entire sequence correct
Delayed Recall
The delayed recall should be performed after 5 minutes have elapsed since the end of the Immediate Recall section.
“Do you remember that list of words I read a few times earlier? Tell me as many words from the list as you can remember in any order.“ Score 1 pt. for each correct response
odified alance rror coring ystem m5 testing
This balance testing is based on a modified version of the Balance Error coring System (BESS)5. A timing device is required for this testing.
Each of -second trial stance is scored by counting the number of errors. The examiner will begin counting errors only after the athlete has assumed the proper start position. The modified BE is calculated by adding one error point for each error during the three -second tests. The maximum number of errors for any single condition is 10. If the athlete commits multiple errors simultaneously, only one error is recorded but the athlete should quickly return to the testing position, and counting should resume once the athlete is set. Athletes that are unable to maintain the testing procedure for a minimum of five seconds at the start are assigned the highest possible score, ten, for that testing condition.
OPTION: For further assessment, the same 3 stances can be performed on a surface of medium density foam (e.g., approximately cm x cm x cm . Balance testing – types of errors
- Hands lifted off 3. Step, stumble, or fall 5. Lifting forefoot or heel iliac crest
4. Moving hip into > 30 6. Remaining out of test
- Opening eyes degrees abduction position > 5 sec
“I am now going to test your balance. Please take your shoes off (if applicable), roll up your pant legs above ankle (if applicable), and remove any ankle taping (if applicable). This test will consist of three twenty second tests with different stances.“ (a) Double leg stance:
“The first stance is standing with your feet together with your hands on your hips and with your eyes closed. You should try to maintain stability in that position for 20 seconds. I will be counting the number of times you move out of this position. I will start timing when you are set and have closed your eyes.“ (b) Single leg stance:
“If you were to kick a ball, which foot would you use? [This will be the dominant foot] Now stand on your non-dominant foot. The dominant leg should be held in approximately 30 degrees of hip flexion and 45 degrees of knee flexion. Again, you should try to maintain stability for 20 seconds with your hands on your hips and your eyes closed. I will be counting the number of times you move out of this position. If you stumble out of this position, open your eyes and return to the start position and continue balancing. I will start timing when you are set and have closed your eyes.“ (c) Tandem stance:
“Now stand heel-to-toe with your non-dominant foot in back. Your weight should be evenly distributed across both feet. Again, you should try to maintain stability for 20 seconds with your hands on your hips and your eyes closed. I will be counting the number of times you move out of this position. If you stumble out of this position, open your eyes and return to the start position and continue balancing. I will start timing when you are set and have closed your eyes.”
Tandem Gait
Participants are instructed to stand with their feet together behind a starting line (the test is best done with footwear removed). Then, they walk in a forward direction as quickly and as accurately as possible along a 38mm wide (sports tape), 3 metre line with an alternate foot heel-to-toe gait ensuring that they approximate their heel and toe on each step. Once they cross the end of the 3m line, they turn 180 degrees and return to the starting point using the same gait. Athletes fail the test if they step off the line, have a separation between their heel and toe, or if they touch or grab the examiner or an object.
Finger to Nose
“I am going to test your coordination now. Please sit comfortably on the chair with your eyes open and your arm (either right or left outstretched (shoulder flexed to degrees and elbow and fingers extended , pointing in front of you. hen I give a start signal, I would like you to perform five successive finger to nose repetitions using your index finger to touch the tip of the nose, and then return to the starting position, as quickly and as accurately as possible.”
References
- c rory et al. onsensus tatement n oncussion In port The th
International Conference On Concussion In Sport Held In Berlin, October 2016. British Journal of Sports Medicine 2017 (available at www.bjsm.bmj.com)
- Maddocks, DL; Dicker, GD; Saling, MM. The assessment of orientation following concussion in athletes. Clinical Journal of Sport Medicine 1995; 5: 32-33
- Jennett, B., Bond, M. Assessment of outcome after severe brain damage: a practical scale. Lancet 1975; i: 480-484
- McCrea M. Standardized mental status testing of acute concussion. Clinical Journal of Sport Medicine. 2001; 11: 176-181
| © Concussion in Sport Group 2017 |
- Guskiewicz KM. Assessment of postural stability following sport-related concussion. Current Sports Medicine Reports. 2003; 2: 24-30
CONCUSSION INFORMATION
Any athlete suspected of having a concussion should be removed from play and seek medical evaluation.
Signs to watch for
roblems could arise over the first – hours. The athlete should not be
left alone and must go to a hospital at once if they experience:
| Worsening headacheDrowsiness or inability to be awakenedInability to recognize people or places | Repeated vomitingUnusual behaviour or confusion or irritable Seizures (arms and legs jerk uncontrollably) | Weakness or numbness in arms or legsUnsteadiness on their feet.Slurred speech |
Consult your physician or licensed healthcare professional after a suspected concussion. Remember, it is better to be safe.
Rest & Rehabilitation
After a concussion, the athlete should have physical rest and relative cognitive rest for a few days to allow their symptoms to improve. In most cases, after no more than a few days of rest, the athlete should gradually increase their daily activity level as long as their symptoms do not worsen. Once the athlete is able to complete their usual daily activities without concussion-related symptoms, the second step of the return to play sport progression can be started. The athlete should not return to play sport until their concussion-related symptoms have resolved and the athlete has successfully returned to full school learning activities.
hen returning to play sport, the athlete should follow a stepwise, medically managed exercise progression, with increasing amounts of exercise. or example:
Graduated Return to Sport Strategy
| Exercise step | unctional exercise at each step | Goal of each step |
| 1. Symptom-limited activity | Daily activities that do not provoke symptoms. | Gradual reintroduction of work school activities. |
| 2. Light aerobic exercise | Walking or stationary cycling at slow to medium pace. No resistance training. | Increase heart rate. |
| 3. port-specific exercise | Running or skating drills. No head impact activities. | Add movement. |
| 4. Non-contact training drills | Harder training drills, e.g., passing drills. May start progressive resistance training. | Exercise, coordination, and increased thinking. |
| 5. Full contact practice | Following medical clearance, participate in normal training activities. | estore confidence and assess functional skills by coaching staff. |
| 6. Return to play sport | Normal game play. |
In this example, it would be typical to have hours (or longer for each step of the progression. If any symptoms worsen while exercising, the athlete should go back to the previous step. Resistance training should be added only in the later stages (Stage 3 or 4 at the earliest).
Written clearance should be provided by a healthcare professional before return to play/sport as directed by local laws and regulations.
Graduated Return to School Strategy
Concussion may affect the ability to learn at school. The athlete may need to miss a few days of school after a concussion. When going back to school, some athletes may need to go back gradually and may need to have some changes made to their schedule so that concussion symptoms do not get worse. If a particular activity makes symptoms worse, then the athlete should stop that activity and rest until symptoms get better. To make sure that the athlete can get back to school without problems, it is important that the healthcare provider, parents, caregivers and teachers talk to each other so that everyone knows what the plan is for the athlete to go back to school.
Note: If mental activity does not cause any symptoms, the athlete may be able to skip step 2 and return to school part-time before doing school activities at home first
| Mental Activity | Activity at each step | Goal of each step |
| 1. Daily activities that do not give the athlete symptoms | Typical activities that the athlete does during the day as long as they do not increase symptoms (e.g. reading, texting, screen time). Start with 5-15 minutes at a time and gradually build up. | Gradual return to typical activities. |
| 2. School activities | Homework, reading or other cognitive activities outside of the classroom. | Increase tolerance to cognitive work. |
| 3. Return to school part-time | Gradual introduction of schoolwork. May need to start with a partial school day or with increased breaks during the day. | Increase academic activities. |
| 4. Return to school full-time | Gradually progress school activities until a full day can be tolerated. | Return to full academic activities and catch up on missed work. |
If the athlete continues to have symptoms with mental activity, some other accomodations that can help with return to school may include:
| Starting school later, only going for half days, or going only to certain classesore time to finish assignments testsuiet room to finish assignments testsNot going to noisy areas like the cafeteria, assembly halls, sporting events, music class, shop class, etc. | Taking lots of breaks during class, homework, testso more than one exam dayShorter assignmentsepetition memory cuesse of a student helper tutorReassurance from teachers that the child will be supported while getting better |
The athlete should not go back to sports until they are back to school/ learning ithout symptoms getting significantly orse and no longer needing any changes to their schedule.
BJSM Online First, published on April 28, 2017 as 10.1136/bjsports-2017-097492childscat5
WHAT IS THE CHILD SCAT5?
The Child SCAT5 is a standardized tool for evaluating concussions designed for use by physicians and licensed healthcare professionals1.
If you are not a physician or licensed healthcare professional, please use the Concussion Recognition Tool 5 (CRT5). The Child SCAT5 is to be used for evaluating Children aged 5 to 12 years. For athletes aged 13 years and older, please use the SCAT5.
Preseason Child SCAT5 baseline testing can be useful for interpreting post-injury test scores, but not required for that purpose. Detailed instructions for use of the Child SCAT5 are provided on page 7. Please read through these instructions carefully before testing the athlete. Brief verbal instructions for each test are given in italics. The only equipment required for the tester is a watch or timer.
This tool may be freely copied in its current form for distribution to individuals, teams, groups and organizations. It should not be altered in any way, re-branded or sold for commercial gain. Any revision, translation or reproduction in a digital form requires specific approval by the Concussion in Sport Group.
Recognise and Remove
A head impact by either a direct blow or indirect transmission of force can be associated with a serious and potentially fatal brain injury. If there are significant concerns, including any of the red flags listed in Box 1, then activation of emergency procedures and urgent transport to the nearest hospital should be arranged.
Key points
- Any athlete with suspected concussion should be REMOVED FROM PLAY, medically assessed and monitored for deterioration. No athlete diagnosed with concussion should be returned to play on the day of injury.
- If the child is suspected of having a concussion and medical personnel are not immediately available, the child should be referred to a medical facility for urgent assessment.
- Concussion signs and symptoms evolve over time and it is important to consider repeat evaluation in the assessment of concussion.
- The diagnosis of a concussion is a clinical judgment, made by a medical professional. The Child SCAT5 should NOT be used by itself to make, or exclude, the diagnosis of concussion. An athlete may have a a concussion even if their Child SCAT5 is “normal”.
Remember:
- The basic principles of first aid (danger, response, airway, breathing, circulation) should be followed.
- Do not attempt to move the athlete (other than that required for airway management) unless trained to do so.
- Assessment for a spinal cord injury is a critical part of the initial on-field assessment.
- Do not remove a helmet or any other equipment unless trained to do so safely.
© Concussion in Sport Group 2017
Copyright Article author (or their employer) 2017. Produced by BMJ Publishing Group Ltd under licence.
CLINICAL NOTES:
Concussion injury advice for the child and parents/carergivers
(To be given to the person monitoring the concussed child)
This child has had an injury to the head and needs to be carefully watched for the next 24 hours by a responsible adult.
If you notice any change in behavior, vomiting, dizziness, worsening headache, double vision or excessive drowsiness, please call an ambulance to take the child to hospital immediately.
Other important points:
Following concussion, the child should rest for at least 24 hours.
- The child should not use a computer, internet or play video games if these activities make symptoms worse.
- The child should not be given any medications, including pain killers, unless prescribed by a medical doctor.
- The child should not go back to school until symptoms are improving.
- The child should not go back to sport or play until a doctor gives permission.
Clinic phone number:
Patient’s name:
Date / time of injury:
Date / time of medical review:
Healthcare Provider:
| INSTRUCTIONS Words in Italics throughout the Child SCAT5 are the instructions given to the athlete by the clinician |
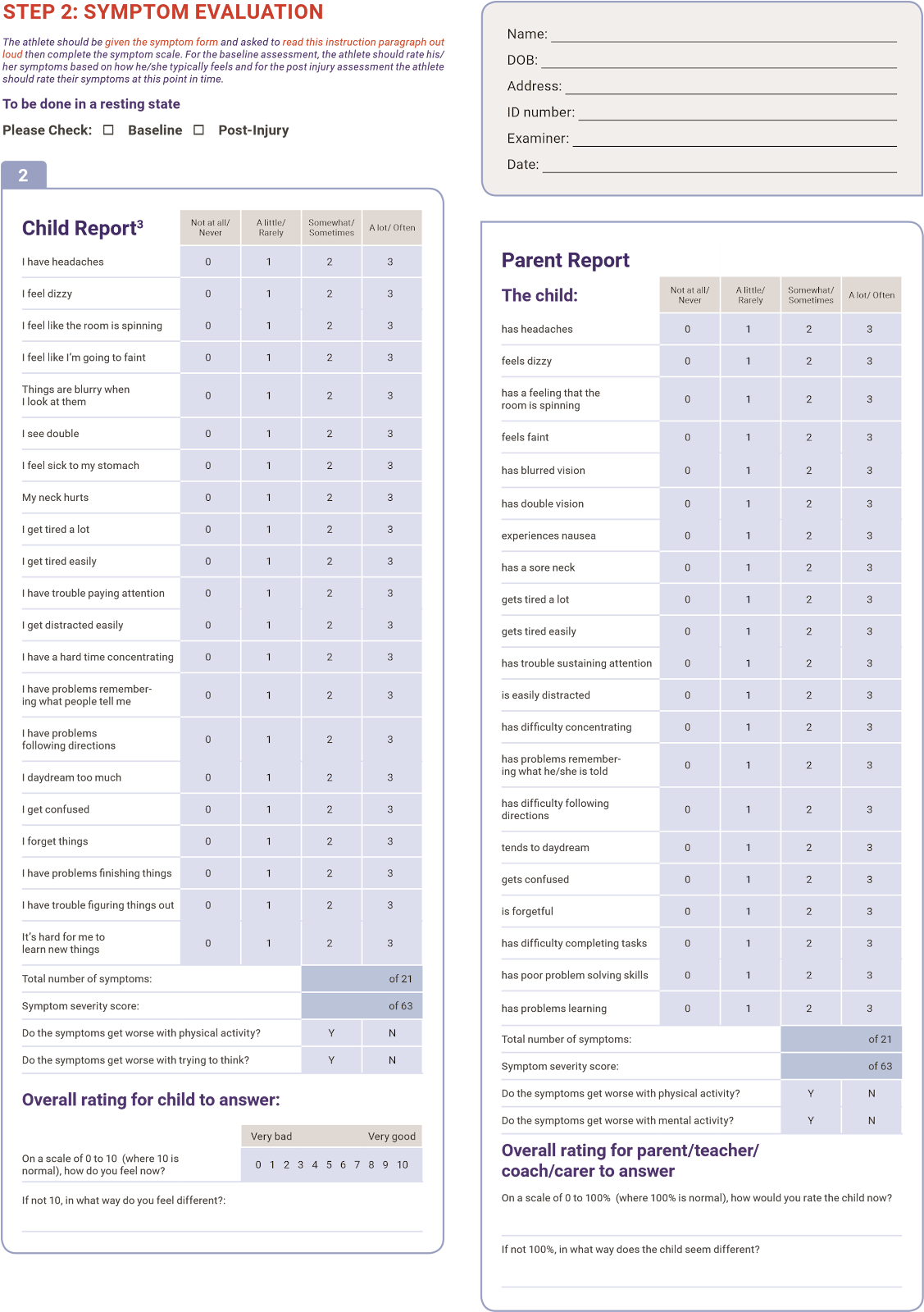
Symptom Scale
In situations where the symptom scale is being completed after exercise, it should still be done in a resting state, at least 10 minutes post exercise.
| At Baseline | On the day of injury | On all subsequent days | |||
| • • | The child is to complete the Child Report, according to how he/ she feels today, andThe parent/carer is to complete the Parent Report according to how the child has been over the previous week. | • • | The child is to complete the Child Report, according to how he/ she feels now. If the parent is present, and has had time to assess the child on the day of injury, the parent completes the Parent Report according to how the child appears now. | • • | The child is to complete the Child Report, according to how he/ she feels today, andThe parent/carer is to complete the Parent Report according to how the child has been over the previous 24 hours. |
For Total number of symptoms, maximum possible is 21
For Symptom severity score, add all scores in table, maximum possible is 21 x 3 = 63
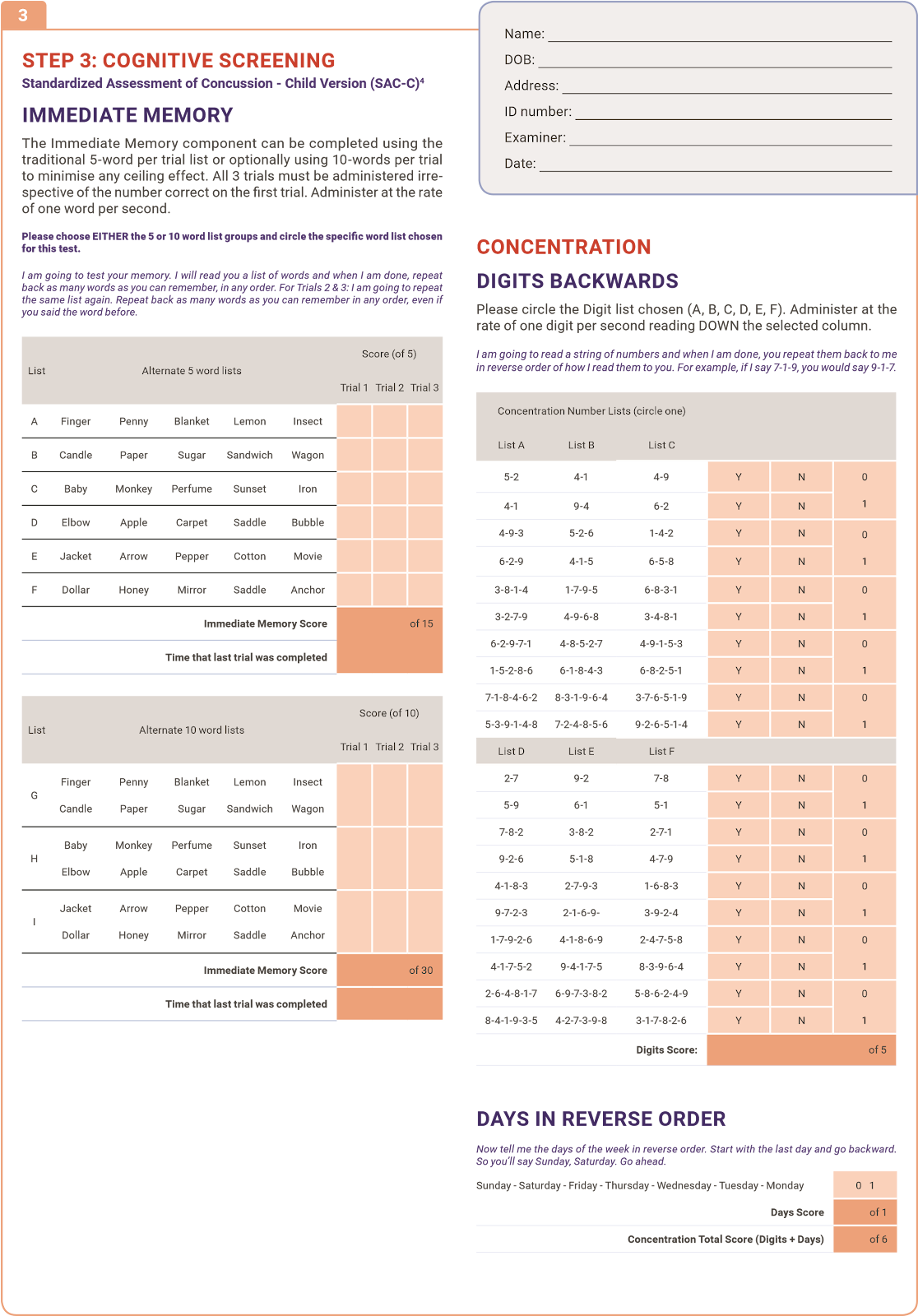
Standardized Assessment of Concussion Child Version (SAC-C) Immediate Memory
Choose one of the 5-word lists. Then perform 3 trials of immediate memory using this list. Complete all 3 trials regardless of score on previous trials.
“I am going to test your memory. I will read you a list of words and when I am done, repeat back as many words as you can remember, in any order.” The words must be read at a rate of one word per second.
OPTION: The literature suggests that the Immediate Memory has a notable ceiling effect when a 5-word list is used. (In younger children, use the 5-word list). In settings where this ceiling is prominent the examiner may wish to make the task more difficult by incorporating two 5–word groups for a total of 10 words per trial. In this case the maximum score per trial is 10 with a total trial maximum of 30.
Trials 2 & 3 MUST be completed regardless of score on trial 1 & 2.
Trials 2 & 3: “I am going to repeat the same list again. Repeat back as many words as you can remember in any order, even if you said the word before.“
Score 1 pt. for each correct response. Total score equals sum across all 3 trials. Do NOT inform the athlete that delayed recall will be tested.
Concentration
Digits backward
Choose one column only, from List A, B, C, D, E or F, and administer those digits as follows:
“I am going to read you some numbers and when I am done, you say them back to me backwards, in reverse order of how I read them to you. For example, if I say 7-1, you would say 1-7.”
If correct, circle “Y” for correct and go to next string length. If incorrect, circle “N” for the first string length and read trial 2 in the same string length. One point possible for each string length. Stop after incorrect on both trials (2 N’s) in a string length. The digits should be read at the rate of one per second.
Days of the week in reverse order
“Now tell me the days of the week in reverse order. Start with Sunday and go backward. So you’ll say Sunday, Saturday … Go ahead”
1 pt. for entire sequence correct
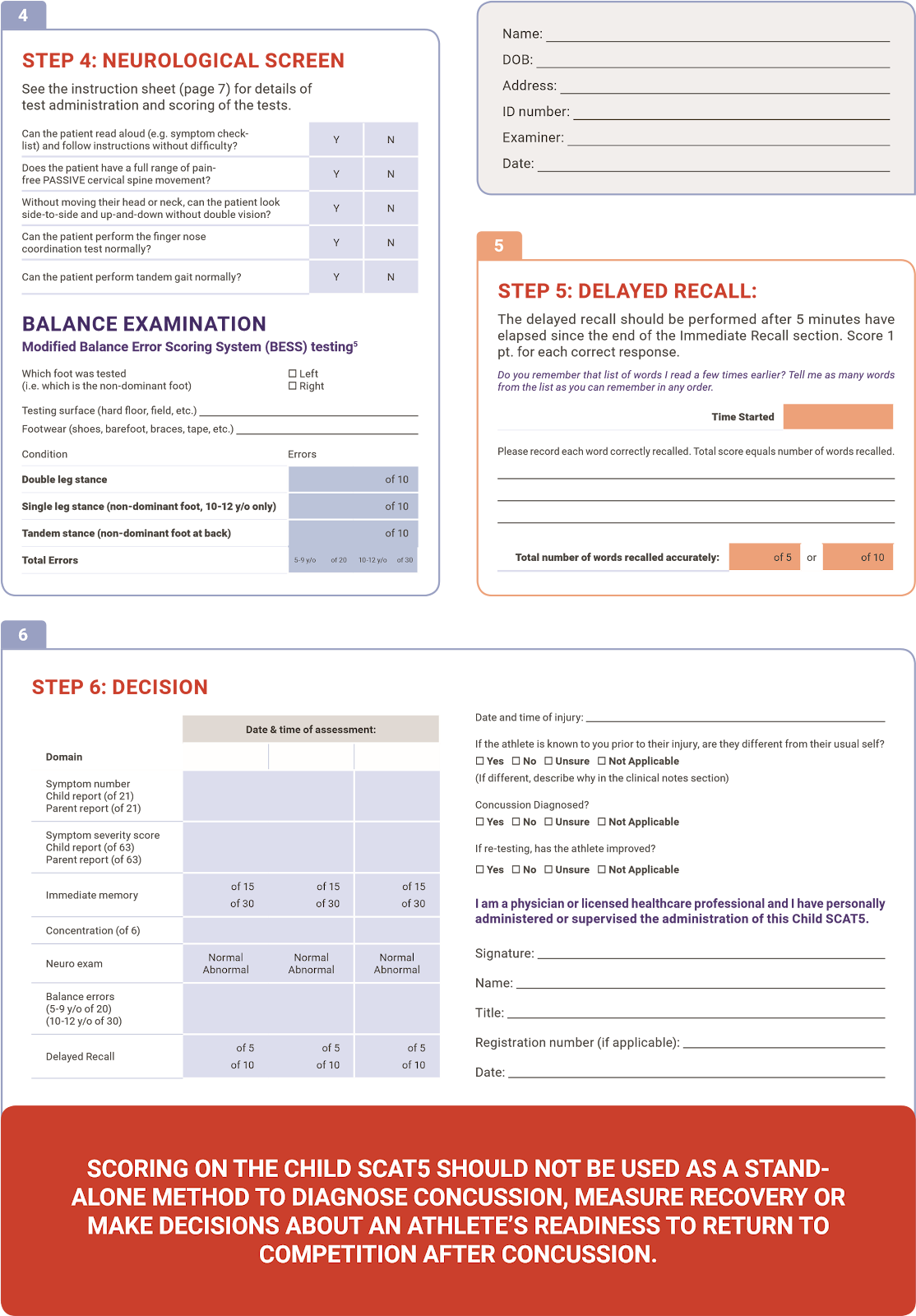
Delayed Recall
The delayed recall should be performed after at least 5 minutes have elapsed since the end of the Immediate Recall section.
“Do you remember that list of words I read a few times earlier? Tell me as many words from the list as you can remember in any order.“
Circle each word correctly recalled. Total score equals number of words recalled.
Neurological Screen Reading
The child is asked to read a paragraph of text from the instructions in the Child SCAT5. For children who can not read, they are asked to describe what they see in a photograph or picture, such as that on page 6 of the Child SCAT5.
Modified Balance Error Scoring System (mBESS)5 testing
These instructions are to be read by the person administering the Child SCAT5, and each balance task should be demonstrated to the child. The child should then be asked to copy what the examiner demonstrated.
Each of 20-second trial/stance is scored by counting the number of errors. The This balance testing is based on a modified version of the Balance Error Scoring System (BESS)5.
A stopwatch or watch with a second hand is required for this testing.
“I am now going to test your balance. Please take your shoes off, roll up your pants above your ankle (if applicable), and remove any ankle taping (if applicable). This test will consist of two different parts.“
OPTION: For further assessment, the same 3 stances can be performed on a surface of medium density foam (e.g., approximately 50cm x 40cm x 6cm).
- Double leg stance:
The first stance is standing with the feet together with hands on hips and with eyes closed. The child should try to maintain stability in that position for 20 seconds. You should inform the child that you will be counting the number of times the child moves out of this position. You should start timing when the child is set and the eyes are closed.
- Tandem stance:
Instruct or show the child how to stand heel-to-toe with the non-dominant foot in the back. Weight should be evenly distributed across both feet. Again, the child should try to maintain stability for 20 seconds with hands on hips and eyes closed. You should inform the child that you will be counting the number of times the child moves out of this position. If the child stumbles out of this position, instruct him/her to open the eyes and return to the start position and continue balancing. You should start timing when the child is set and the eyes are closed.
- Single leg stance (10-12 year olds only):
“If you were to kick a ball, which foot would you use? [This will be the dominant foot] Now stand on your other foot. You should bend your other leg and hold it up (show the child). Again, try to stay in that position for 20 seconds with your hands on your hips and your eyes closed. I will be counting the number of times you move out of this position. If you move out of this position, open your eyes and return to the start position and keep balancing. I will start timing when you are set and have closed your eyes.“
Balance testing – types of errors
| Hands lifted off iliac crestOpening eyes | Step, stumble, or fallMoving hip into > 30 degrees abduction | Lifting forefoot or heelRemaining out of test position > 5 sec |
Each of the 20-second trials is scored by counting the errors, or deviations from the proper stance, accumulated by the child. The examiner will begin counting errors only after the child has assumed the proper start position. The modified BESS is calculated by adding one error point for each error during the 20-second tests. The maximum total number of errors for any single condition is 10. If a child commits multiple errors simultaneously, only one error is recorded but the child should quickly return to the testing position, and counting should resume once subject is set. Children who are unable to maintain the testing procedure for a minimum of five seconds at the start are assigned the highest possible score, ten, for that testing condition.
Tandem Gait
Instruction for the examiner – Demonstrate the following to the child:
The child is instructed to stand with their feet together behind a starting line (the test is best done with footwear removed). Then, they walk in a forward direction as quickly and as accurately as possible along a 38mm wide (sports tape), 3 metre line with an alternate foot heel-to-toe gait ensuring that they approximate their heel and toe on each step. Once they cross the end of the 3m line, they turn 180 degrees and return to the starting point using the same gait. Children fail the test if they step off the line, have a separation between their heel and toe, or if they touch or grab the examiner or an object.
Finger to Nose
The tester should demonstrate it to the child.
“I am going to test your coordination now. Please sit comfortably on the chair with your eyes open and your arm (either right or left) outstretched (shoulder flexed to 90 degrees and elbow and fingers extended). When I give a start signal, I would like you to perform five successive finger to nose repetitions using your index finger to touch the tip of the nose as quickly and as accurately as possible.”
Scoring: 5 correct repetitions in < 4 seconds = 1
Note for testers: Children fail the test if they do not touch their nose, do not fully extend their elbow or do not perform five repetitions.
References
- McCrory et al. Consensus Statement On Concussion In Sport – The 5th International Conference On Concussion In Sport Held In Berlin, October 2016. British Journal of Sports Medicine 2017 (available at www.bjsm.bmj.com)
- Jennett, B., Bond, M. Assessment of outcome after severe brain damage: a practical scale. Lancet 1975; i: 480-484
- Ayr, L.K., Yeates, K.O., Taylor, H.G., Brown, M. Dimensions of postconcussive symptoms in children with mild traumatic brain injuries. Journal of the International Neuropsychological Society. 2009; 15:19–30
- McCrea M. Standardized mental status testing of acute concussion. Clinical Journal of Sports Medicine. 2001; 11: 176-181
- Guskiewicz KM. Assessment of postural stability following sport-related concussion.
| © Concussion in Sport Group 2017 |
Current Sports Medicine Reports. 2003; 2: 24-30
CONCUSSION INFORMATION
If you think you or a teammate has a concussion, tell your coach/trainer/ parent right away so that you can be taken out of the game. You or your teammate should be seen by a doctor as soon as possible. YOU OR YOUR TEAMMATE SHOULD NOT GO BACK TO PLAY/SPORT THAT DAY.
Signs to watch for
Problems can happen over the first 24-48 hours. You or your teammate should not be left alone and must go to a hospital right away if any of the following happens:
| New headache, or headache gets worseNeck pain that gets worseBecomes sleepy/ drowsy or can’t be woken upCannot recognise people or places | Feeling sick to your • Has weakness, stomach or vomiting numbness or tingling (arms, legs or face)Acting weird/strange, seems/feels confused, • Is unsteady walking or is irritable or standingHas any seizures • Talking is slurred (arms and/or legs jerk uncontrollably) • Cannot understand what someone is saying or directions |
Consult your physician or licensed healthcare professional after a suspected concussion. Remember, it is better to be safe. Graduated Return to Sport Strategy
After a concussion, the child should rest physically and mentally for a few days to allow symptoms to get better. In most cases, after a few days of rest, they can gradually increase their daily activity level as long as symptoms don’t get worse. Once they are able to do their usual daily activities without symptoms, the child should gradually increase exercise in steps, guided by the healthcare professional (see below).
The athlete should not return to play/sport the day of injury.
NOTE: An initial period of a few days of both cognitive (“thinking”) and physical rest is recommended before beginning the Return to Sport progression.
| Exercise step | Functional exercise at each step | Goal of each step |
| 1. Symptom-limited activity | Daily activities that do not provoke symptoms. | Gradual reintroduction of work/school activities. |
| 2. Light aerobic exercise | Walking or stationary cycling at slow to medium pace. No resistance training. | Increase heart rate. |
| 3. Sport-specific exercise | Running or skating drills. No head impact activities. | Add movement. |
| 4. Non-contact training drills | Harder training drills, e.g., passing drills. May start progressive resistance training. | Exercise, coordination, and increased thinking. |
| 5. Full contact practice | Following medical clearance, participate in normal training activities. | Restore confidence and assess functional skills by coaching staff. |
| 6. Return to play/sport | Normal game play. |
There should be at least 24 hours (or longer) for each step of the progression. If any symptoms worsen while exercising, the athlete should go back to the previous step. Resistance training should be added only in the later stages (Stage 3 or 4 at the earliest). The athlete should not return to sport until the concussion symptoms have gone, they have successfully returned to full school/learning activities, and the healthcare professional has given the child written permission to return to sport.
If the child has symptoms for more than a month, they should ask to be referred to a healthcare professional who is an expert in the management of concussion.
Graduated Return to School Strategy
Concussion may affect the ability to learn at school. The child may need to miss a few days of school after a concussion, but the child’s doctor should help them get back to school after a few days. When going back to school, some children may need to go back gradually and may need to have some changes made to their schedule so that concussion symptoms don’t get a lot worse. If a particular activity makes symptoms a lot worse, then the child should stop that activity and rest until symptoms get better. To make sure that the child can get back to school without problems, it is important that the health care provider, parents/caregivers and teachers talk to each other so that everyone knows what the plan is for the child to go back to school.
Note: If mental activity does not cause any symptoms, the child may be able to return to school part-time without doing school activities at home first.
| Mental Activity | Activity at each step | Goal of each step |
| 1. Daily activities that do not give the child symptoms | Typical activities that the child does during the day as long as they do not increase symptoms (e.g. reading, texting, screen time). Start with 5-15 minutes at a time and gradually build up. | Gradual return to typical activities. |
| 2. School activities | Homework, reading or other cognitive activities outside of the classroom. | Increase tolerance to cognitive work. |
| 3. Return to school part-time | Gradual introduction of schoolwork. May need to start with a partial school day or with increased breaks during the day. | Increase academic activities. |
| 4. Return to school full-time | Gradually progress school activities until a full day can be tolerated. | Return to full academic activities and catch up on missed work. |
If the child continues to have symptoms with mental activity, some other things that can be done to help with return to school may include:
| Starting school later, only going for half days, or going only to certain classesMore time to finish assignments/testsQuiet room to finish assignments/testsNot going to noisy areas like the cafeteria, assembly halls, sporting events, music class, shop class, etc. | Taking lots of breaks during class, homework, testsNo more than one exam/dayShorter assignmentsRepetition/memory cuesUse of a student helper/tutorReassurance from teachers that the child will be supported while getting better |
The child should not go back to sports until they are back to school/ learning, without symptoms getting significantly worse and no longer needing any changes to their schedule.
© Concussion in Sport Group 2017
Sport concussion assessment tool for childrens ages 5 to 12 years
Br J Sports Med published online April 26, 2017
| Updated information and services can be found at: http://bjsm.bmj.com/content/early/2017/04/28/bjsports-2017-097492c hildscat5.citation | |
| These include: | |
| Email alerting service | Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article. |
Notes
To request permissions go to: http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
